OHIP billing is complex. DoctorCare alleviates the administrative burden of billing management by identifying missed and potential revenue opportunities and enabling you to quickly and easily resolve outstanding errors, monitor your roster, and capitalize on all of your revenue opportunities.
Pain-free billing review, submissions, and management.
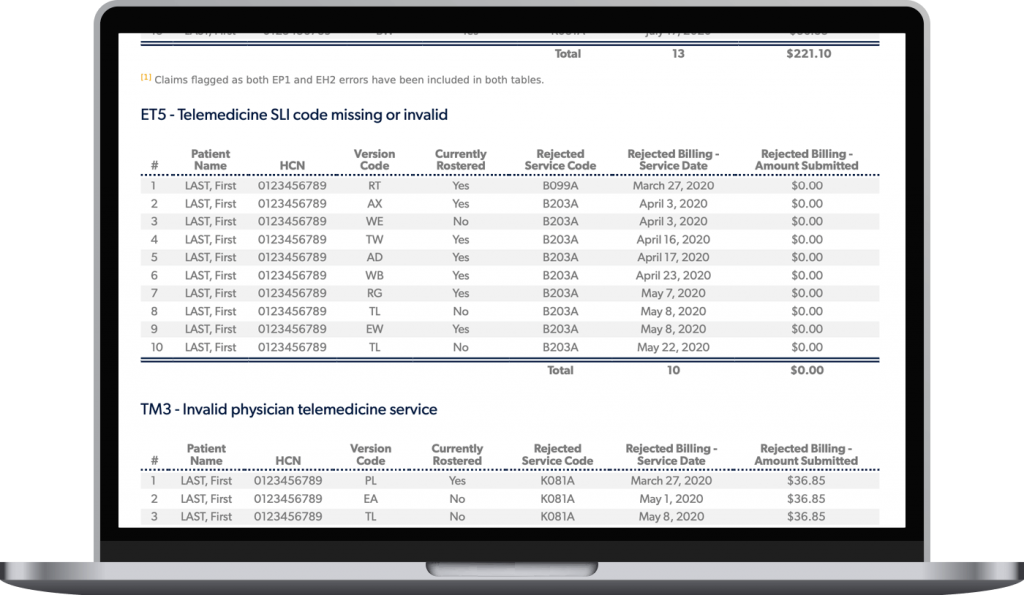
Resolve outstanding OHIP billing errors and automate re-submissions.
Gain insight into your billing performance, understand how you get paid, and key drivers of revenue.
Actively monitor your roster, get alerts on patient visit frequency, and get outside use under control.
Get help to interpret and capitalize on your access bonuses, special premiums, and diabetic management.
Stay on top of your preventive care bonus and improve patient screening rates.
FHO and FHG group practice requirements make OHIP billing and bonus achievements an increasingly complicated process. DoctorCare presents your billing information and makes recommendations, including your top priorities, in an easy to review format. We can then automate your billings, taking one more thing off your plate.

As a busy specialist, you don’t have time to spend on the administrative burden of medical billing and could miss out on getting paid for your hard work. With Trillium Medical Billing, a DoctorCare company, we bring 35 years of hands-on, personalized medical billing experience to ensure accurate billings and maximum revenue, recovering an average of $30,000.
The implementation of the Physician Services Agreement (PSA) marked a significant step towards addressing crucial issues that both patients and physicians encounter, thereby fostering continual enhancement of the healthcare system. We’ve helped physicians stay updated on the latest changes and educate them on the new billing requirements under the agreement. Read our resources for the latest updates on the PSA.
© 2022 DoctorCare. All rights reserved. |
In just a couple of hours we can get you started with optimizing your billings and maximizing your revenue.
Please fill out our contact form and we will get in touch with you shortly.
We may send you periodic emails about news and events. We respect your inbox and you can unsubscribe at any time.
In just a couple of hours we can get you started with optimizing your billings and maximizing your revenue.
Please fill out our contact form and we will get in touch with you shortly.
We may send you periodic emails about news and events. We respect your inbox and you can unsubscribe at any time.